Glaucoma Treatment Options
A. Medical Therapy
Medical treatment is the first line treatment for most type of glaucoma. There are few glaucoma/pressure lowering eyedrops which work in different mechanism; either reducing production of fluid in the eye or/and promoting drainage of fluid from the eye.
Prostaglandin Analogs
[ Latanoprost (Xalatan), Travoprost (Travatan), Bimatoprost (Lumigan), Tafluprost (Taflutan) ]
These are the first-class medical therapy in term of efficacy. They reduce eye pressure by enhancing the drainage of fluid (aqueous) from the eye. Studies shows prostaglandin analogs were able to reduce eye pressure by 30% to 35%. Dosing is once daily at bedtime.
Possible side effects are eye redness, elongation and darkening of eyelashes and skin around the eye.
Beta-Blockers (timolol, betaxolol)
They lower the eye pressure about 20% to 30% by decreasing the amount of fluid produced in the eye. Timolol has once a day and twice a day dosing while Betaxolol is used twice a day.
Complications are dry eyes, cornea erosion and more systemic side effects compared to Prostaglandin group.
Betoptic is a selective beta-blocker. It is less effective in lowering the eye pressure, but have less side effects on pulse rate, heart, and lungs.
Timolol is non-selective beta-blocker which could lower the eye pressure more compares to selective blockers. However, they should not be used in patients with: asthma, severe heart failure or lung disease, bradycardia. They can also cause depression and impotence for male.
Alpha-Agonists (Brimonidine, Alphagan-P, Iopidine)
Eye pressure is lowered by decreasing the amount of aqueous humor produced and also by promoting outflow of fluid. They are class-2 medication in term of effectiveness.
Dosing is twice or three times daily.
The common side effects are redness and itchiness of the eye which occurs in 20-30% of patients. It is not suitable for children for its sedative effect.
Carbonic Anhydrase Inhibitors (Diamox©, or Azopt or Trusopt©)
This groups of eye pressure lowering agents act by reducing the secretion of aqueous humor. The eyedrops are Azopt and Trusopts. Both can cause stinging or burning sensation in the eyes for a while after application. Other side effects are bitter taste, itchy and redness.
Diamox is very potent in lowering the eye pressure by decreasing the amount of aqueous humor made. It can be taken as a pill or by intravenous infusion twice to four times a day.
However, it comes with a lot of side effects. These include fatigue, loss of appetite, metabolic acidosis, kidney stones and depression. These are sulfa drugs -- so it is contra-indicated for people who are allergic to medications. It can also cause aplastic anaemia which can be life threatening. Diamox is usually given temporarily to lower eye pressure before the schedule of Glaucoma Surgery.
Miotics (pilocarpine, carbachol)
Is the oldest class of medications used for the treatment of glaucoma. They work by increasing the drainage of fluid from the eye. It can be given at various dosing intervals varying between once weekly to four times daily.
Most side effects are limited to the eye. They make your pupil smaller which can make your vision seem dimmer. Headache is a common problem.
Omidenepag isopropyl ophthalmic solution 0.002% (EYBELIS®)
Is a selective prostaglandin E2 receptor 2 agonist with a non-prostaglandin structure. It was approved in 2018 in Japan for treatment of Glaucoma and ocular hypertension but is only recommended to glaucoma patients who have no previous cataract surgeries.
Its eye pressure lowering effect is as good as Prostaglandin Analogs. However it would not leads to darkening of eyelids and sunken eyes like Prostaglandin Analogs do. Side effects are usually mild red or dry eyes.
Rho Kinase Inhibitors (Ripasudil (Glanatec Ophthalmic Solution 0.4%)
Ripasudil is recently launched topical eyedrops. It had undergone clinical trials in Japan and proven efficacious with many potential medical benefits to the eyes.
It reduces eye pressure by increasing the drainage of aqueous via trabecular meshwork and Schlemm’s canal. It also enhances the outflow through the uveo-scleral route; the unconventional pathway. Clinical trials had showed that Ripasudil could lower eye pressure in almost all glaucoma subtypes.
Common side effects are red eyes which usually resolves within 2 hours after application. Other possible side effects are allergic conjunctivitis and blepharitis.
B. Laser Therapy
Different Laser treatments work in different type of glaucoma.
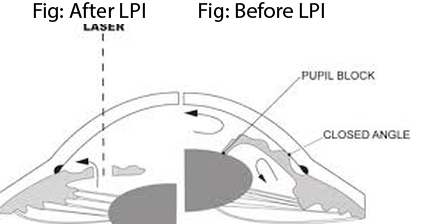
Laser Peripheral Iridotomy (LPI)
Acute Angle closure glaucoma can be treated with emergency Laser Peripheral Iridotomy (LPI) or Laser Iridoplasty procedure. This laser procedure creates a ‘bypass’ to facilitate fluid flow and to open-up the angle/drainage site of the eye.
It is the definitive emergency treatment when patient come to Hospital Emergency Room with severe eye pain and visual loss. Severe headache associated with nausea and vomiting is common. The presentation could be mis-interpreted as ‘Migaine Attack’ or ‘Acute Gastritis’. Very often patients with severe headache were wrongly referred to Neuro Surgery to rule out brain tumour (MRI Brain) and those had nausea and vomiting to Gastroenterologist. The sudden rise of eye pressure could go up to 50-70 mmHg and this could result in blindness just within a few hours.
|
|
|
 *picture obtained from google images |
|||
|
|
After emergency Laser Peripheral Iridotomy, the eye pressure usually could be lowered effectively. The cornea swelling would subside with treatment and resume its clarity. However, patient’s vision hardly get back to normal because the pupil may remain dilated due to iris muscle/sphincter damage and also there is already some degree of optic nerve damage.
Sometimes, The eye pressure could not be lowered even after emergency Laser Peripheral Iridotomy. This is usually because the lens bulk is too huge and is pressing on the already narrow angle of the eye. In some instances; the lens/cataract already subluxated. In that case, an emergency lens extraction (cataract surgery) is warranted. Cataract surgery in this bad stage is technically challenging and difficult.
Patients’ vision outcome depends on how high his/her eye pressure on presentation, duration of the ‘unattended’ high eye pressure and degree of optic nerve damage. Vision may be lost instantly or may not recover fully (with eye pressure lowered with treatment) following a acute angle closure attack.
Prophylactic/Preventive Laser Peripheral Iridotomy should be done in eye with narrow angle detected during eye examination/screening. This is to prevent acute angle closure glaucoma. Optic nerve damage and visual loss can be prevented.
|
|
Laser trabeculoplasty
Laser trabeculoplasty is a laser procedure on primary open angle glaucoma which targets on the trabecular meshwork to stimulate/ increase the outflow of aqueous thereby reduce the eye pressure/IOP.
There are different lasers to perform trabeculoplasty, including “Argon” or “Selective laser trabeculoplasty”.
It is important to note that this procedure is not always effective; success rate is about 70%. It may work for a limited period of time; a few months or few years. When effective, the IOP lowering effect is mild to moderate which is about 20-30% reduction of eye pressure from the baseline.
After the laser, the patient should maintain regular follow-up, and may still require eyedrops or surgery.
Angle Closure Glaucoma and Secondary Glaucoma like Uveitic Glaucoma, Rubeotic/Neovascular Glaucoma and Glaucoma secondary to eye injury are not suitable cases for this mode of treatment.
Fig: Laser is being aimed at the trabecular meshwork
Laser cyclophotocoagulation
This laser procedure aims to decrease the aqueous production by treating part of the ciliary body (tissue behind the iris responsible to produce aqueous humor).
This procedure is usually reserved for eyes with end stage glaucoma with poor vision, where the IOP is high despite maximum topical eyedrops or failed surgical treatment. It is also indicated in painful blind eyes. The possible side effects are eye inflammation and eye globe atrophy/shrinkage.
Now, a new laser device using ‘Micropulse’ is less destructive and it can be applied to patients with good vision. However its success rate is around 70% and repeat treatment may be needed.
Other device using endoscopic technique is called ‘Endo-Cyclophotocoagulation’. It is an invasive surgical technique where incision on the eyeball is needed to allow introduction of the laser probe near to the ciliary body. Like any intraocular surgical procedure; it comes with risk of eye infections and blindness besides risk of laser treatment like eye inflammation and eye globe atrophy.
C. Glaucoma Surgery
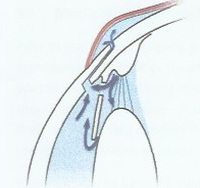
i. Trabeculectomy
This surgical procedure is to lower the eye prressure and thus prevent further damage to the optic nerve/loss of vision in glaucoma.
This procedure usually performed under local anesthesia. My surgical technique adheres to Moorfield Safe Surgery System. It involves making a small hole in the eye wall/sclera to drain the aquoeus from inside the eye a small reservoir (bleb) under the skin of the eye (conjunctiva). During the surgery, Mitomycin C (anti-scarring agent) may be applied on the eye surface for 2-3 minutes to reduce scarring. Post-operative follow-up is intensive where patients need to be seen weekly for the first 4 weeks post-operative period. Sutures may be removed to lower the eye pressure and additional subconjunctiva injection of steroid with/without 5-Flurouracil (anti-scarring agent) to counteract the eye’s natural healing/ scarring response. Scarring prevents the trabeculectomy from draining aquoeus in long term.
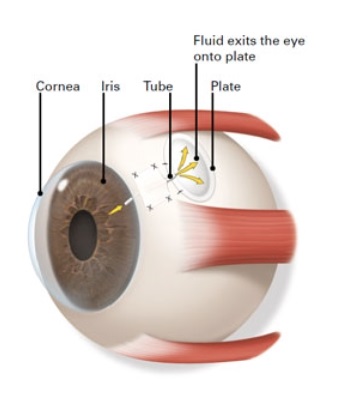
ii. Glaucoma Tube Shunt Surgery with Glaucoma Drainage Devices
This type of eye surgery involve implantatiom of Glaucoma Drainage device on the eye surface with an aquoeus shunts to drain the fluid (aquoeus) from inside the eye. This is to lower the eye pressure to prevent further damage to the optic nerve.The two commonly used Glaucoma Drainage Devices are Baerveldt Glaucoma Implant and Ahmed Glaucoma Valve.These devices are made up of a small silicone tube attached to a plate. The silicone tube is to be inserted into the eye to drain the aquoeus to a plate that sits on the surface of the eyeball. A donor sclera/ cornea patch is used to cover and keep the device in place. There are many types of Glaucoma drainage devices with different sizes and designs available; eg. Baervelt, Ahmed Valve or Clear Path, Molteno and Paul Glaucoma Implant.
iii. Minimally Invasive Glaucoma Surgery
Minimal Invasive Glaucoma Surgery (MIGS) constitutes a group of surgical interventions which offer safe and quick surgery with minimal tissue disruption, and thus allow rapid recovery for the patients.
MIGS works by increase aqueous outflow/drainage inside the eye and thus help to reduce intra-ocular pressure(IOP). Some MIGS decreases aqueous production by laser ablation of the ciliary body (structure that produce aqueous).
Up to todate, there are few MIGS been registered for use in Malaysia eg. i-stent, i-Stent Inject G2, i-Stent Inject Gw, Xen Gel Stent, Kahook blade, Trabectome and Micropulse Diode laser and Endocyclophotocoagulation. Some MIGS are indicated for use in Primary Open Angle Glaucoma only, while some can be used for one or more types of glaucoma.
MIGS are usually indicated for Glaucoma of mild or moderate severity because of its limited efficacy in IOP reduction. Some MIGS procedures are performed in combination with cataract surgery; for eg i-Stent trabecular micro-bypass and Hydrus Stent. Eye pressure reduction for i-Stent and Hydrus are about 10 - 40 % according to published clinical trials and this had allowed reduction of number of topical eyedrops required to stabilize the disease.
Studies showed that early surgical intervention with some minimally invasive glaucoma devices would help slow down the progression of Glaucoma and reduce the likelihood of needing incisional Glaucoma Surgeries in future. Currently, MIGS are still very highly priced and their cost-effectiveness (cost to lower every 1 mmHg of IOP) need to be studied further.
It is important to emphasize that MIGS are not the treatment choices for patients with more advanced glaucoma who require extensive IOP reduction (eg IOP > 30 mmHg) or very low target IOP (eg IOP 10 mmHg). Traditional incisional surgeries - glaucoma drainage implants or trabeculectomy are still the gold standard for effective IOP reduction especially for the advanced Glaucoma or those with uncontrolled high IOP.
Treatment for each Glaucoma patient should be tailored and individualized. It depends on type of glaucoma, target IOP, patients’ visual prognosis, life expectancy and general health conditions. Do consult a Glaucoma Specialist on your treatment plan.
Is ‘Stem Cell Transplant’ available for glaucoma treatment?
Can stem cell transplant be done to repair the damaged optic nerve in glaucoma? This treatment is currently still in the experimental stage and is not possible for glaucoma patients yet. Scientists are still working on it, and hopefully stem cell transplant may be a reality in future.